INFORMATION ON BREAST CANCER
Cancer Awareness,Blog
1. What is Breast Cancer?
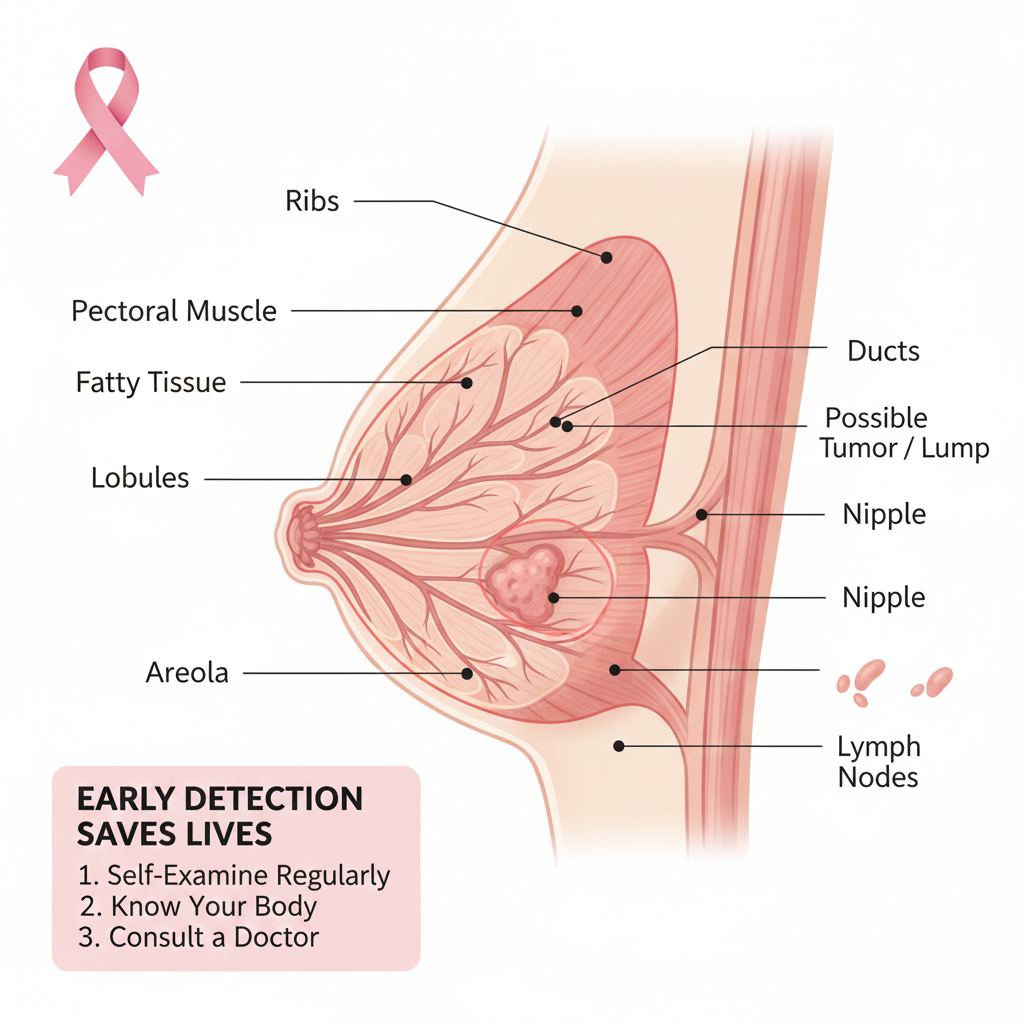
Breast cancer develops when the cells in the breast begin to grow abnormally and multiply uncontrollably. These cells usually form a lump or mass and can invade nearby tissues or spread (metastasize) to other parts of the body. Most breast cancers start either in the milk ducts (ductal carcinoma) or in the lobules (lobular carcinoma). It can occur in both women and men, though it is far more common in women.
2. What are the risk factors for breast cancer?
Having one or more risk factors does not necessarily mean you will get breast cancer. Many women with breast cancer have no known risk factors apart from age and gender.
- Gender: Women are about 100 times more likely to develop breast cancer than men.
- Aging: The risk increases with age. About 1 in 8 breast cancers occur in women younger than 45, whereas 2 in 3 occur in women aged 55 or older.
- Genetic Factors: Inherited mutations such as BRCA1 or BRCA2 genes
- Family History: Having a mother, sister, or daughter with breast cancer increases the risk.
- Reproductive and Hormonal Factors: Early menstruation, late menopause, or never having children may increase risk.
- Lifestyle Factors: Obesity, lack of exercise, excessive alcohol use, and a high-fat diet can contribute to risk.
- Radiation Exposure: Prior radiation therapy to the chest area, especially at a young age, increases risk.
3. What are the signs and symptoms of breast cancer?
The most common symptom is a new lump or mass in the breast or underarm. A hard, irregular, and painless lump is more likely to be cancerous, but not always. Some cancers can feel soft, tender, or even painful. Hence, any new lump should be checked by a healthcare professional experienced in breast diseases.
Other possible symptoms include:
- Swelling of part or all of the breast (even without a distinct lump)
- Skin dimpling or puckering
- Pain in the breast or nipple
- Nipple turning inward (retraction)
- Redness, scaling, or thickening of nipple or breast skin
- Nipple discharge, which may be clear, milky, or blood-stained
4. What is breast self-examination?
Breast self-examination is a simple method by which you can check your own breasts to stay aware of any early signs of breast cancer.
- Use your eyes and hands to observe any change in the size, shape, or texture of your breasts.
- If you notice any unusual changes, such as a lump, swelling, skin dimpling, or nipple discharge or if one breast feels different from the other, inform your doctor promptly.
- Remember, not all breast changes are due to cancer; other benign (non-cancerous) conditions can also cause such changes.
Common ways to perform Breast Self-Examination:
- While lying down: Lie on your back on a bed or flat surface. When lying down, the breast tissue spreads evenly, making it easier to feel for any lumps or thickening.
- While bathing: Apply soap on your fingers and breasts so that your fingers can glide smoothly over the skin, helping you detect any unusual changes.
5. Can breast cancer be found early?
Yes. Early detection greatly improves treatment success and survival. Screening tests are designed to identify breast cancer before symptoms appear.
Recommended screening methods include:
- Clinical Breast Examination (CBE): Performed by a trained healthcare provider to check for lumps or changes. Please start from age of 30years once a year
- Mammography: A specialized X-ray that can detect very small cancers not felt on examination. Please start from age of 40 years once a year
- Some women at higher risk may be advised to undergo breast MRI or genetic testing.
6. How is breast cancer treated?
Treatment depends on the type, stage, receptor status, and overall health of the patient. It often involves a combination of therapies planned by a multidisciplinary team of doctors.
The main types of treatment are:
Surgery:
- Breast-conserving surgery (lumpectomy) – removal of the tumour with a small margin of normal tissue.
- Mastectomy – removal of the entire breast.
- Lymph nodes from the armpit (axilla) may also be removed to check for spread.
Radiation Therapy:
- Uses high-energy rays to destroy remaining cancer cells after surgery.
Chemotherapy:
- Uses anti-cancer drugs to kill cancer cells, often before or after surgery.
Hormone Therapy:
- For cancers that are oestrogen or progesterone receptor positive (ER/PR+).
Targeted Therapy:
- For HER2-positive cancers (e.g., trastuzumab, pertuzumab).
Bone-Directed Therapy:
- Used to strengthen bones and reduce complications if the cancer has spread to bone.
7. What should you ask your doctor about breast cancer?
It is important to have an open and honest discussion with your treating team. Some useful questions include:
- What type and stage of breast cancer do I have?
- Has my cancer spread to lymph nodes or other organs?
- Do I need additional tests before starting treatment?
- What treatment options are available for my stage?
- Should I undergo genetic testing or consider a clinical trial?
- What are the possible side effects of treatment?
- Will I need breast reconstruction, and when should it be done?
- How long will my treatment last, and where will it be done?
- What diet and lifestyle changes should I follow during and after treatment?
- What are the chances of recurrence, and how will it be monitored?
- Will treatment affect my ability to have children or cause menopause?
8. What Happens After Treatment for Breast Cancer?
Once treatment is completed, you will enter a follow-up phase. These visits help your doctors monitor for recurrence, manage side effects, and provide emotional and physical support.
Follow-up schedule:
- Every 3–6 months for the first 2–3 years
- Every 6–12 months for the next few years
- Then once a year after 5 years
- If you had breast-conserving surgery, a mammogram will be done about 6 months after radiation, and then annually.
- Women who had mastectomy should continue annual mammograms on the remaining breast.
9. What is Lymphedema after breast cancer treatment?
Lymphedema is swelling of the arm or hand due to fluid build-up after lymph node removal or radiation. Early signs include tightness, heaviness, or swelling in the arm or chest wall on the operated side.
Tips to prevent or manage lymphedema:
- Avoid pricks and needles on the arm on the operated side.
- Blood pressure measurement should be avoided on the side of surgery.
- Heavy weights more than 5 kg should not be lifted by the arm on the operated side.
- Cuts, stings, insect bite should be avoided.
- Tight garments, bracelets and rings should not be worn on the affected side.
- Be careful while paring your nails. Avoid waxing of the arm on the affected side.
- In case of any accidental cuts, wash wound carefully and apply antiseptic ointment at once.
- If there is redness or swelling in the arm, report back immediately to your treating physician.
- If you wish to undertake a trip by flight, kindly ensure you have an arm sleeve (custom made) for the arm on the operated side during the duration of the flight. Information regarding the same will be provided to you at the hospital.
- No blood sugar testing to be done from operated side
- Keep the skin clean and moisturized.
- Maintain a healthy body weight.
- Gentle arm exercises and physiotherapy may help improve lymph flow.











