PATIENT INFORMATION ON RECTAL CANCER
Cancer Awareness
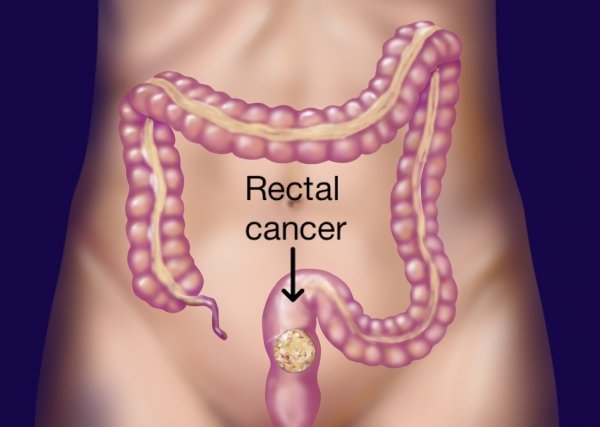
What is the Rectum? Where is it located?
The rectum and anal canal forms the lower end of the
body’s digestive system. The digestive system is made up of the esophagus,
stomach, small and large intestine. The main part of the large intestine is called the colon, which is about 150 cm long. This is split into four sections: the ascending, transverse, descending and sigmoid colon. Some water and salts are absorbed into the body from the colon. The colon leads into the rectum (back passage), which is about 15 cm long and is contained in the pelvis. Within the pelvis the rectum is located just in front of the sacrum (i.e. the lower portion of the backbone) with the urinary bladder and prostate in front of it in males. In females, the uterus and vagina lie in between the urinary bladder in front and the rectum behind. The rectum stores feces (stools) before they are passed out from the anus.
Why have I developed rectal cancer?
Development of rectal cancer cannot be attributed to any single factor. There are certain risk factors which increase the chance of developing rectal cancer. Risk factors include:
- Age – Rectal cancer is more common in older people (50 and above). There has been reported to be an increased incidence of rectal cancer in young Indians. It is unclear at the current time if such an incidence is just a relative increase owing to our larger population as compared to Western countries. Irrespective of this, the importance of awareness that even the young may be afflicted with rectal cancer needs to be born in mind and they should seek medical attention if they encounter the symptoms listed below
- A person with one or more family members with bowel cancer
- A personal history of cancer of the colon, ovary, endometrium or breast
- A history of ulcerative colitis (conditions of the colon) for more than 8-10 years
- Obesity
- Lifestyle factors – little exercise, drinking lot of alcohol, and long-term use of tobacco
- Certain hereditary conditions such as familial adenomatous polyposis, hereditary nonpolyposis colorectal cancer (HNPCC, Lynch syndrome)
However, patients
may develop these cancers even without any of these risk factors being present.
What are the symptoms of rectal cancer?
The symptoms of rectal cancer include but are not limited to the following:
- A change in bowel habits – unexplained diarrhoea or constipation
- Blood (either bright red or very dark) in the stool
- Feeling that the bowel does not empty completely after a bowel motion
- Frequent gas pains, bloating, fullness or cramps
- Unexplained weight loss
- Feeling very tired.
All patients above the age of 40 years are advised to have a faecal occult blood test every 6 months. If positive, the patent is sent for a colonoscopy. It is advisable for adults above the age of 40 years, especially those with a family history of bowel cancer, to get themselves tested for faecal occult blood by visiting their family physician.
Certain benign conditions of the lower rectum and anus
like piles (haemorrhoids), anal fissure (wound in the anal canal) etc. can also
present with symptoms similar to rectal cancer. It is important to rule out
rectal cancer in patients with these benign conditions as sometimes both can be
present. If the cancer spreads to other parts of the body, various other
symptoms can develop. The symptoms depend on where it has spread to. All the
above symptoms can be due to other conditions, so tests are needed to confirm
rectal cancer.
What investigations will
I be subjected to?
The best investigation to diagnose rectal cancer is endoscopy
with a biopsy of the tumour. As cancer of the rectum may be associated with the
simultaneous presence of tumours in another portion of the large intestine,
colonoscopy should be performed to evaluate the entire large bowel. A computed
tomography (CT) scan or Magnetic resonance imaging (MRI) of the abdomen and
pelvis will help to support the diagnosis of the cancer as well to determine
whether the cancer is at an early stage or whether it has spread to the lymph
nodes, liver or other organs and if the rectal cancer has infiltrated the
surrounding organs. Serum
Are there different
types of rectal cancer?
Yes, there are different types of rectal cancer depending on the type of cell / tissue from which the cancer is arising. Adenocarcinoma is the most common type of rectal cancer. Gastrointestinal stromal tumours (GIST), lymphoma and leiomyoma are some of the less common types of rectal cancers. The treatment depends on the type of cancer.
Is cancer of the anal
canal similar to rectal cancer?
Although the anal canal is situated below the rectum and forms the last 4cm of the body's digestive system, cancer of the anal canal is quite different from rectal cancer. The most common form of anal cancer is squamous cell carcinoma although other forms like melanoma also occur in this region. These cancers tend to spread to the lymph nodes in the groin unlike rectal cancer which spreads in an upward direction towards the abdominal lymph nodes. Unlike rectal cancer, the majority of patients with anal cancer are controlled with a treatment combination of radiation and chemotherapy. However patients who are not controlled with this treatment may require an abdomino-perineal resection. (details of this procedure have been mentioned below)
At what stage is the cancer?
Pre-operative investigations give some information about the stage of the disease, however the most accurate staging of rectal cancer is based on histopathology and is possible only after surgery when the removed cancer and the draining lymph nodes are examined by the pathologist.
Rectal cancer can be broadly classified into:
Stage 1 / Early cancer –
cancer only within the rectum with no spread of disease outside it.
Stage 2 or 3 / Locally advanced cancer – when the cancer appears large and/or invading other surrounding
organs, with enlarged lymph nodes.
Stage 4 / Metastatic
– when the cancer has spread far from the rectum e.g. to the liver, lungs, etc.
These patients also usually have some fluid building up in the abdomen. It is
usually not possible to cure stage 4 cancer. Treatment is intended to reduce
symptoms and improve the patient’s quality of life.
If the cancer comes back after initial treatment, it is known as recurrent cancer.
Now that I have been
diagnosed to have rectal cancer, how will I be treated?
A team of multi-disciplinary specialists including a surgeon, medical gastroenterologists, radiation and medical oncologist, radiologist and pathologist will discuss the treatment that would be best for you. Different types of treatment are available for patients with rectal cancer. Four types of standard treatment are used:
- Surgery
- Chemotherapy
- Radiation therapy
- Targeted Therapy
The type of treatment administered depends on the stage
of disease in each patient. For early stage disease surgery is usually offered
first. Following the operation and depending on the pathology report,
additional treatment in the form of radiation, or chemotherapy or both could be
required.
Patients with locally advanced rectal cancer tend to do better with a combination of radiation and chemotherapy prior to surgery and this order of treatment i.e. Chemotherapy ± radiation followed by surgery, is usually offered wherever possible. A gap of at least six weeks is required between radiation and surgery. Additional chemotherapy may be required following surgery in some patients.
Patients with metastatic disease need chemotherapy with or without targeted therapy. Surgery may also be required in these patients at some point. Chemotherapy is a cancer treatment that uses drugs to stop the growth of cancer cells either by killing the cells or stopping them from dividing. Radiation therapy is a cancer treatment that uses high energy X-rays or other types of radiation to kill cancer cells or to keep them from growing. Targeted therapy uses drugs or substances to identify and attack specific cancer cells without harming normal cells.
Which kind of surgery is
done for rectal cancer?
The type of surgery largely depends on the location of the cancer from the anal opening.
For tumours very close to the anus, the anal canal cannot be preserved and the entire rectum and anus needs to be removed to eliminate all cancerous tissue. The place where the anus was, is closed permanently and the patient is then given a permanent stoma (i.e. an opening in the skin through which the intestine empties its contents into a bag) in the left lower part of the abdomen. This operation is known as an abdomino-perineal resection (APR).
In patients where the cancer does not extend right upto
the anus, the portion of rectum with the cancerous tissue is removed and the
descending colon is joined to the remaining rectum to preserve the normal
intestinal continuity. This operation is known as an anterior resection.
Patients in whom an anterior resection is performed sometimes need a temporary
stoma to divert the stools until the area where the intestine was joined has
completely healed.
For some tumours which are very close but do not reach the anus, the decision between an abdomino-perineal resection and anterior resection will have to be made during the operation. The patient needs to be prepared for both procedures before surgery.
If I have a temporary stoma when will it be
closed?
The temporary stoma is usually closed after complete healing of the area where the intestine was joined. This usually takes 6 weeks to 3 months. However, if the patient requires additional treatment after surgery in the form of chemotherapy or radiotherapy or both, the temporary stoma is only closed after all treatment is completed. This may take up to a year in some patients.
Do I need another
operation to close the stoma?
Yes, another operation will be required to close the stoma. This is also a major operation but not quite as major as the first one where the cancer was removed.
Will I be able to lead
a normal life after rectal cancer surgery?
If the cancer is controlled with treatment i.e. surgery, radiation and chemotherapy, then patients usually lead a normal life following rectal surgery. However, depending on the procedure performed a few changes will have to be made. Patients having an APR will have to learn how to manage their stoma. There is a dedicated stoma management team to help these patients. In patients receiving an anterior resection, as the rectum is removed there is no space for the body to collect the stools. Therefore, immediately after the surgery patients will experience more frequent bowel motions and may have some difficulty in controlling the passage of stools. However, over time the body adjusts and the frequency of stools decreases and continence improves.
What is laparoscopic surgery? Can it be used for
rectal cancer?
Laparoscopy, also known as key hole surgery, is a surgical technique where the operation is performed through small holes in the abdominal wall using specialized instruments. Some patients also have an incision in the abdomen but this is usually of smaller size as compared to conventional open surgery. Rectal cancer surgery can be performed laparoscopically but must be done at centres equipped with the instruments and expertise for it. Laparoscopy has been shown to offer benefits to the patients in terms of less pain, a faster return of bowel function, and a shorter hospital stay. However every laparoscopic procedure has the possibility of being converted to the conventional open approach if the entire procedure cannot be completed laparoscopically.
Can patients
have sexual dysfunction following rectal cancer surgery?
As the rectum lies in the pelvis, it lies very close to the nerves that supply the sexual organs. These nerves are very fine and are at risk of injury during surgery. Although every attempt is made to safeguard these nerves some patients do experience sexual dysfunction in the form of impotence (i.e. failure of erection), retrograde ejaculation (i.e. failure of ejaculation) or dyspareunia (painful sexual intercourse in females). In some of these patients the sexual function improves over time but some patients do have persistent sexual dysfunction that may be life-long.
Are there any alternatives besides surgery?
Till date, curative surgery offers the best results in terms of local control and overall survival for rectal cancer.
How do I prepare myself for surgery?
The preparation is generally similar to any major
surgery. If you are a smoker it is absolutely essential to stop smoking.
Breathing exercises using the incentive spirometer and football bladder should
be started. Follow the anaesthetist’s advice regarding continuation of
medications if you are on any. A high protein diet is preferred to improve
nutrition.
How major is the surgery? What are the possible complications?
Rectal surgeries are deemed as major procedures with a risk of complications (<1>
The complications of rectal resection (removal of the rectum and lymph nodes and joining back (anastomosis) the healthy bowel / intestine) include:
- Leak of anastomosis
- Bleeding from the anastomosis
- Bladder complications
- Sexual dysfunction.
For how long do I stay in the hospital?
In an uncomplicated case, hospital stay after surgery is 7-10 days. This may be longer when there are complications.
Will I need any further treatment after surgery?
The decision about treatment is based on the final histopathology report which will be available approximately 7-10 days following surgery. If any of the lymph nodes are positive and your general condition is good enough then you may be referred to the medical (GI) oncologist for consideration for chemotherapy, radiotherapy or both. The aim of treatment after surgery is to get rid of any remaining cancer cells which may not be seen on scans thereby reducing the chance of cancer coming back in the future.
What will be my survival after surgery? Are there any chances of the
cancer coming back?
The survival depends on the stage of the disease. The
average 5-year survival for all stages after curative surgery for colorectal
cancer is between 40-75?pending on the stage of the cancer. To-date, there
is no fool-proof way of predicting which patients will have recurrence and
which patient will not.
Are there any special precautions I need to take to prevent cancer from coming back?
There are no proven precautions, but it is logical to exercise regularly, avoid using tobacco, drink alcohol in moderation and maintain a good diet.
How frequently should I follow up after surgery?
After completion of treatment you will be advised to follow-up
once in 3-4 months in the first 2 years. Then the frequency will be reduced to once
in 6 months for the next 3 years. Subsequent follow up will be once a year.
During each follow-up you will be asked to do certain blood tests, especially