PATIENT INFORMATION ON LUNG CANCER
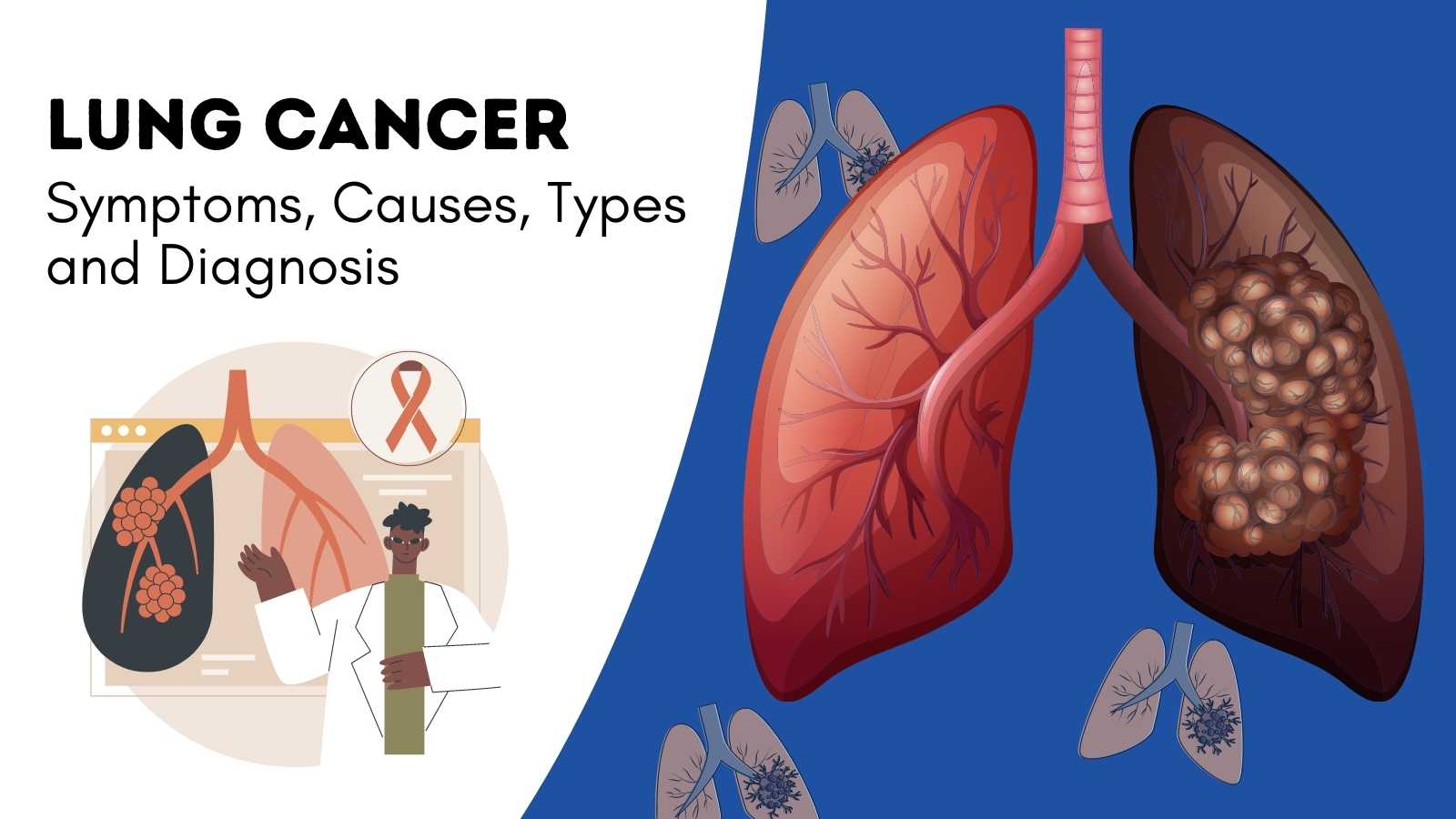
Cancer Awareness
What
is lung cancer?
Lung cancer is an abnormal growth of cells in the lungs. Lung cancer may eventually spread to other parts of the body if not discovered and treated early.
What are the risk factors for lung cancer?
Smoking is the single greatest avoidable risk factor for cancer. It is responsible for one in four of all deaths from cancer. Smoking causes around 90% of lung cancers. There are multiple benefits from quitting. Once you stop smoking, your risk of lung cancer starts to go down. 10 years after you've given up, your lung cancer risk is about half that of a smoker.
What causes lung cancer?
The most significant cause of lung cancer is cigarette smoke (National Cancer Institute). Roughly 85% of lung cancers are diagnosed in former or current smokers; other cases may be caused by environmental exposure to materials like radon, asbestos or uranium, or second hand smoke. Genetics can also play a role.
I have been smoking for many years?
Why should I stop smoking now?
Lung cancer takes years to develop. The risk increases with each year of smoking, and with each cigarette smoked per day. Stopping smoking will reduce the risk of lung cancer developing as well as reduce the likelihood of developing heart and lung problems. Smoking also increases the risk of other diseases, such as chronic lung disease, heart disease, stroke and other cancers such as head and neck cancers. Smoking can also harm your spouse and family members.
Do
non-smokers get lung cancer?
Yes, non-smokers can get lung cancer, but the risk is much lower than in smokers. There are factors other than smoking that increase a person's risk of getting lung cancer. Breathing in other people's smoke, exposure to radon, asbestos, air pollution, certain chemicals in the workplace, and a personal or family history of lung cancer are also risk factors for lung cancer.
What
lung cancer risks are associated with second hand smoke?
Second hand smoke contains twice as much tar and nicotine per unit volume than smoke inhaled directly from a cigarette. More significantly, second hand smoke contains three times more cancer-causing compounds and 30 times more carbon monoxide than first hand smoke. Second hand smoke is responsible for thousands of cases of lung cancer and asthma each year.
Why
is early lung cancer screening important?
It is important because lung cancer has no symptoms in its early stages. Over 85% of men and women diagnosed with lung cancer today are diagnosed in later stages, after symptoms have occurred and when there is very little chance of cure. Consequently, approximately 95% of people diagnosed each year die from the disease.
What
are the most common symptoms of lung cancer?
This is a tricky one because sometimes
there aren't any symptoms of lung cancer. One in four people don’t even
have symptoms when their lung cancer is advanced. In other people, symptoms
that may suggest lung cancer can include:
- Shortness of breath
- Coughing that doesn't go away
- Wheezing
- Coughing up blood
- Chest pain
- Fever
- Weight loss
What are the tests for lung cancer?
There are a number of tests that can be used to detect lung cancer. However,
most tests miss many early cancers, and are often ordered only after the
patient has started having symptoms. Traditional lung cancer tests include:
- Chest x-ray
- Sputum Cytology (analyzing cells in mucus)
- Bronchoscopy (using a tube through the mouth to look at the lungs with a tiny camera).
To confirm that a person has lung cancer, the doctor must examine fluid or tissue from the lung. This is done through a biopsy - the removal of a small sample of fluid or tissue for examination under a microscope by a pathologist. A biopsy can show whether a person has cancer. A number of procedures may be used to obtain this tissue.
Bronchoscopy -- The doctor puts a bronchoscope - a thin, lighted tube into the mouth or nose and down through the windpipe to look into the breathing passages. Through this tube, the doctor can collect cells or small samples of tissue.
Needle Aspiration - The doctor numbs the chest area and inserts a thin needle into the tumor to remove a sample of tissue.
Thoracentesis - Using a needle, the doctor removes a sample of the fluid that surrounds the lungs to check for cancer cells.
Thoracotomy - Surgery to open the chest is sometimes needed to diagnose lung cancer. This procedure is a major operation performed in a hospital.
PET-CT– An imaging test that uses a radioactive substance (called a tracer) to look for cancer cells in the lungs.
What
are the standard treatments for lung cancer?
Surgery is an operation to remove
the cancer. Depending on the location of the tumour, the surgeon may remove a
small part of the lung, a lobe of the lung, or the entire lung.
Conventional chemotherapy uses
anti-cancer drugs to kill cancer cells throughout the body. Doctors use
chemotherapy to control cancer growth and relieve symptoms. Anti-cancer drugs
are given by injection; through a catheter, a long thin tube temporarily placed
in a large vein; or in pill form.
Targeted agents and Immunotherapy are a newer class of drugs that are designed to act against specific weaknesses in cancer cells or surrounding supportive tissues, such as blood vessels. These drugs can also be taken by pill or by IV. They are most effective in cancers with specific changes in their genes.
Radiation therapy uses high-energy beams to kill cancer cells and shrink tumors. An external machine delivers radiation to a limited area, affecting cancer cells only in that area. Doctors may use radiation therapy before surgery to shrink a tumor or after surgery to destroy any cancer cells remaining in the treated area.
What
are the treatment options for the lung cancer that has spread to other parts of
the body?
Almost 60-70% of patients have advanced lung cancer. Additional tests on the biopsy specimen to subtype the cancer may help determine whether chemotherapy or targeted therapy is more suitable. The treatment goal in such cases is to enhance the quality of life, reduce symptoms, and prolong survival. Currently, patients in this category are not only living longer but also enjoying a better quality of life.
What
types of surgery are used to treat lung cancer?
Depending on the extent of the cancer, the surgeon may decide to remove part or all of the lung. Taking out a part of the lobe of a lung is called a segmental or wedge resection. If a lobectomy is performed, an entire lobe of the lung is removed; this is usually the preferred surgery for lung cancer if it can be done. A pneumonectomy involves the removal of an entire lung, while a sleeve resection removes only the part of the bronchus with cancer, with the lung then reattached to the remaining part of the bronchus
After
a lung is removed, what happens to the space that's left in the chest?
Space left after surgery is filled up with body fluid and scar tissue and the other lung usually expands. Until this happens, there may be a feeling of emptiness on the side of the operation.
Can
I breathe and live normally if I have a lung removed?
Most likely, depending on your lung function before the surgery. The removal of one or two lobes may limit strenuous physical exercise, but you should otherwise be able to breathe and live normally. If you have an entire lung removed, you may experience shortness of breath during exertion, but at rest, your breathing will be normal. Breathing exercises will help you in adapting to this.
How
can lung cancer be prevented?
The best way to prevent lung cancer is
to avoid smoking and to avoid breathing in other people's smoke. If you smoke,
quit. While the risk for former smokers remains elevated when compared to a
non-smoker, it continues to fall with each year of smoking cessation. In fact,
10 years after you've given up, your lung cancer risk is about half that of a
smoker.
There is some evidence that eating a
healthy diet rich in fibre, fruit and vegetables may help reduce
the risk of lung cancer. Also, as per research, higher levels of physical
activity may lead to a 20-40% reduction in lung cancer risk.