INFORMATION ON OESOPHAGUS (FOODPIPE) CANCER
Cancer Awareness
What is Oesophagus Cancer?
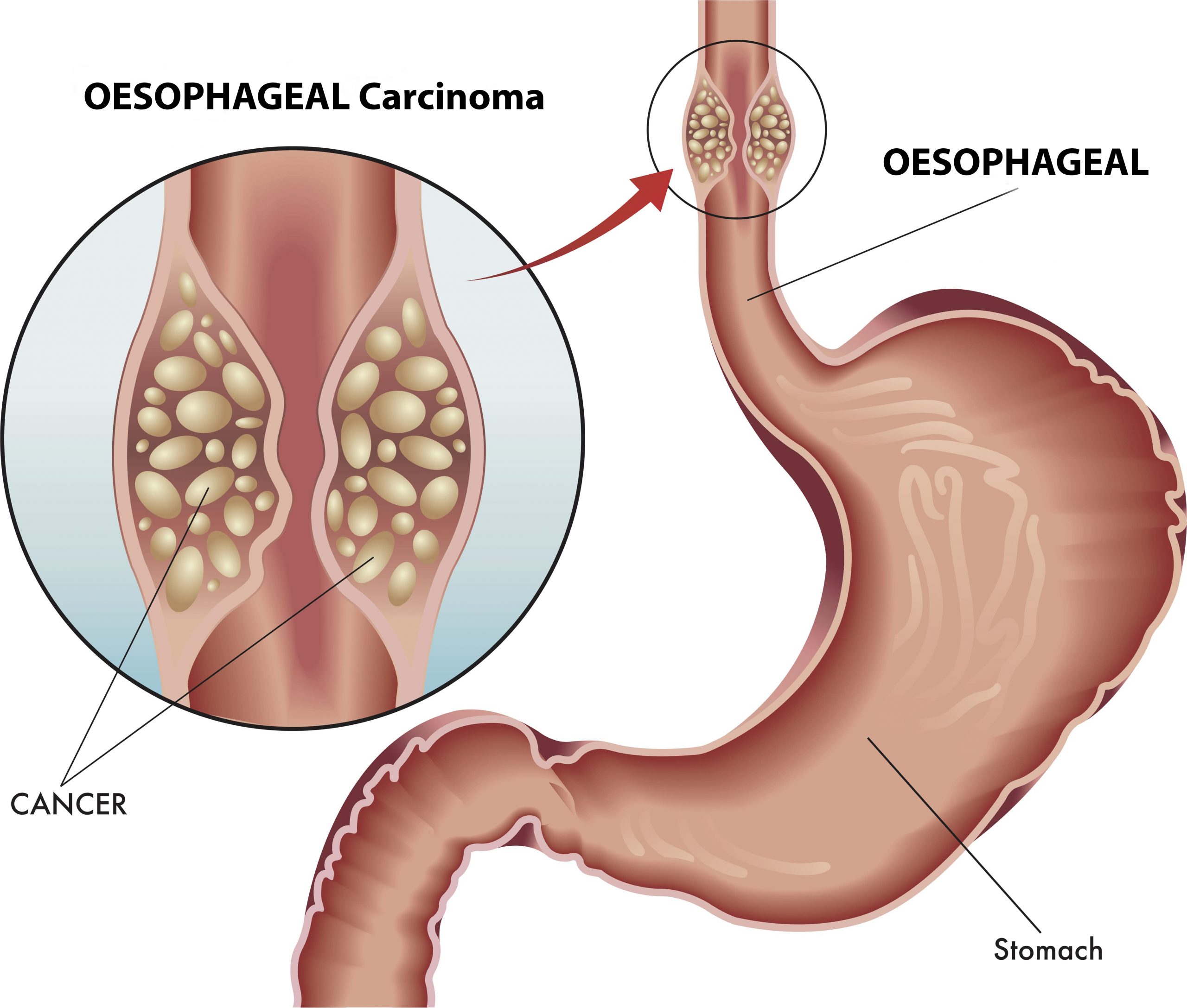
Oesophagus, also known as the food pipe is a
muscular tube measuring 20-25 cm long and 2-3 cm wide that serves as a conduit
for moving food and drink from the mouth to the stomach. The
oesophagus is divided into 3 parts and
cancers may arise in any of thee parts. The type of surgery and treatment will
depend on the location of the tumour. Oesophageal cancer is the 6th most
common cancer in India.
Cancers that start in the area where the oesophagus joins the stomach (the gastro-esophageal junction) including about the first 2 inches of the stomach tend to behave like esophageal cancers; they are grouped with esophageal cancers.
Why have I developed Oesophagus
cancer?
Development of oesophageal cancer cannot be attributed to any single factor. There are multiple factors suggested to be responsible for causing oesophageal cancer. These include diet, smoking, long-term acid reflux, alcohol /tobacco consumption and obesity. High intake of salted, pickled or smoked foods, very hot drinks, as well as dried fish and meat and refined carbohydrates significantly increase the risk of developing oesophageal cancer.. However, patients may develop these cancers even without any of these risk factors being present.
What are the symptoms of
oesophagus cancer?
The presentation of oesophageal cancer can be with any of the following symptoms : Difficulty in swallowing food (dysphagia), Unexplained weight loss, Worsening indigestion or heartburn, Tightness or pain in the chest, Cough or hoarseness of voice. Patients, who present with heart-burn and reflux for the first time after the age of 40 years, need to undergo an endoscopy to rule out cancer amongst other causes. Lump in the abdomen and back pain are late signs of the disease and usually indicate an advanced disease.
What investigations will
I be subjected to?
The best investigation to diagnose oesophagus cancer is endoscopy with a biopsy of the tumour. A computed tomography (CT) scan of the abdomen and pelvis will help to support the diagnosis of the cancer as well to determine whether the cancer is at an early stage or whether it has spread to the lymph nodes, liver or other organs and if the stomach cancer has infiltrated the surrounding organs. Liver function tests, X-ray of the chest, etc. are other investigations to decide the stage of the disease. If an operation is being planned, some more tests may be necessary to decide fitness of the patient for general anaesthesia. Endoscopic ultrasound (using an ultrasound probe at the end of an endoscope) helps the doctor to see the extent of growth of tumor into nearby areas as well as to check for enlarged lymph nodes.
Are there different
types of oesophagus cancer?
Yes, there are different types of oesophagus cancer depending on the
type of cell / tissue from which the cancer is arising. squamous cell carcinoma
arises from the stratified squamous epithelial lining of the organ, and
adenocarcinoma affecting columnar glandular cells that replace the squamous
epithelium. Other types of esophageal cancer are uncommon. The treatment
depends on the type of cancer.
At what stage is the
cancer?
Accurate staging of the
cancer is based on histopathology and will be possible only after surgery.
Based on clinical and radiological findings, oesophagus cancer can be broadly
classified into:
Stage 1 / Early cancer – cancer only
within the oesophagus with no spread of
disease outside of it
Stage 2 or 3 / Locally advanced cancer –
when the cancer appears large and or/ invading other surrounding organs, with
enlarged lymph nodes
Stage 4 / Metastatic – when the cancer
has spread far from the oesophagus, for eg to the liver, lungs, brain, ovary,
etc.
If the cancer comes back after initial treatment, it is known as recurrent cancer.
Now that I have been
diagnosed to have oesophagus cancer, how will I be treated?
A team of multi-disciplinary specialists including a surgeon,
medical gastroenterologists, radiation and medical oncologist, radiologist and
pathologist will discuss the treatment that would be best for you. The
treatment is usually decided based on the stage of the disease and in early
cancer the optimal treatment will be surgery. In locally advanced tumors, the
treatment will be with chemotherapy or chemo-radiotherapy first. If the cancer
responds well and shrinks, surgery may be offered after this treatment.
In metastatic / advanced tumours, the treatment is usually
chemotherapy or treatment directed towards controlling the symptoms
(symptomatic care).
In some patients, a stent may have to be inserted especially if there is difficulty in swallowing leading to vomiting.
Which kind of surgery is
done for oesophageal cancer?
The type of surgery depends on the location of the cancer and
extent. Removal of a portion of the oesophagus is called oesophagectomy.
Curative surgeries are done with an aim to remove the entire cancer
with a margin of normal tissue around and all the lymph nodes involved
(lymphadenectomy).
Lymph nodes around the oesophagus
are removed at the same time to check if cancer cells have spread into
them.
Laparoscopic / key-hole surgery has been used in some centres around the world to perform surgery. However, its value in terms of ability to completely remove the cancer and the lymph nodes as compared to open surgery are still unclear at the present time.
Palliative surgery is done for symptom control and not with intent for cure. This is because these surgeries are done in patients with advanced disease who have developed complications of the cancer. Sometimes, even if a patient is taken up for emergency surgery due to a complication of the cancer, no resection may be possible if the disease is very advanced and the abdomen will just have to be closed without any further surgical intervention. In some patients with an obstruction who are not fit for surgery, endoscopic stenting of the tumour may be attempted.
Are there any
alternatives besides surgery?
Till date, surgery is the only proven curative option for oesophageal cancer. In some instances, chemo-radiotherapy is effective is squamous cell cancers.
How do I prepare myself
for surgery?
The preparation is generally similar to any major surgery. If you are a smoker it is absolutely essential to stop smoking. Breathing exercises using the incentive spirometer and football bladder should be started. Follow the anaesthetist’s advice regarding continuation of medications if you are on any. A high protein diet is preferred to improve nutrition.
How major is the
surgery? What are the possible complications?
Oesophagectomy with lymphadenectomy is deemed as major surgeries with a risk of complications (4-10%) and a very small risk of death (<2>This means that if 100 people are operated, less than 2 of them have a chance of death. The complications of Oesophagectomy (removal of the oesophagus and lymph nodes and joining back (anastomosis) the healthy bowel / intestine) include:
- Leak of anastomosis
- Bleeding from the anastomosis
- Prolonged vomiting
For how long do I stay
in the hospital?
In an uncomplicated case, hospital stay after surgery is 9-14 days.
This may be longer when there are complications.
Will I need any further
treatment after surgery?
The decision about
adjuvant treatment is based on the final histopathology report which will be
available approximately 7-10 days following surgery. If any of the lymph nodes
are positive and your general condition is good enough then you may be referred
to the medical (GI) oncologist for consideration for chemotherapy or targeted
therapy in some cases.
What will be my survival after surgery? Are there any chances of the cancer coming back?
The survival depends on the stage of the disease. The average 5-year
survival after curative surgery for oesophagus cancer is 25-35%. This means that 25-35 out of
a 100 people with oesophagus cancer will
survive and be disease-free at the end of 5 years. As of date there is no
foolproof way of predicting which patients will have recurrence and which
patient will not.
Are there any special
precautions I need to take to prevent cancer from coming back?
There are no
proven precautions, but it is logical to exercise regularly, avoid using
tobacco and alcohol, and maintain a good diet. Following oesophagectomy, you may need to eat smaller meals at regular intervals.
How frequently should I follow up after surgery?
After completion of
treatment you will be advised to follow-up once in 3-4 months in the first 2-3
years. Then the frequency will be reduced to once in 6 months for the next 2-3
years. Subsequent follow up will be once a year. During each follow-up you will
be asked to do certain blood tests. You may also be advised to get an
ultrasound of the abdomen done.